The Core Role of Plantar Pressure Plate in Predicting Diabetic Foot Ulcers
The plantar pressure plate, through precise measurement and analysis of the pressure distribution, peak values, and variation patterns of the plantar regions of diabetic patients during standing and walking, provides critical and objective biomechanical evidence for predicting ulcer risk. Its core value is reflected in the following aspects:
Identifying High-Risk Areas (Locating the “Time Bomb”):
Accurate Hotspot Mapping: In dynamic walking states, the pressure plate can generate a detailed plantar pressure distribution map (usually a heat map). It intuitively shows which areas are subjected to abnormally high pressure (such as beneath the metatarsal heads, heel, or bony prominences of deformities).
Quantifying Key Parameters: It not only shows the location, but also precisely measures the peak pressure (instantaneous maximum pressure value) and pressure–time integral (the total amount of pressure sustained). These two parameters are among the most important indicators for predicting ulcers. Repeated and persistent high pressure or prolonged pressure duration will directly cause ischemia and micro-damage to the skin and tissues, eventually developing into ulcers.
Beyond Subjective Perception: Due to diabetic neuropathy, patients usually cannot feel these abnormal high pressures. The pressure plate provides objective, quantitative data, compensating for the risk blind spot caused by sensory loss.
Quantifying Gait Abnormalities (Revealing the Root of Risk):
Abnormal Foot Morphology and Force Line: Diabetes-related joint motion restriction (such as ankle dorsiflexion limitation), muscle atrophy (intrinsic foot muscles) can lead to foot deformities (hammer toe, claw toe, Charcot foot, etc.) and altered force lines (such as varus or valgus). The pressure plate can capture how these changes lead to abnormal pressure distribution shifts (e.g., excessive medial or lateral bias).
Center of Pressure (COP) Trajectory Analysis: Analyzing the movement trajectory of the plantar center of pressure during walking. The COP trajectory of patients with diabetic neuropathy or balance disorders is often unstable, irregular, with increased range of deviation or asymmetry. This not only increases the risk of falling, but also reflects poor foot control, resulting in localized pressure concentration or abnormal impact forces.
Changes in Gait Characteristics: It can analyze variations in stance phase duration, stride length, walking speed, etc. Abnormal gait patterns are often the body’s adaptations or compensatory mechanisms to pain, deformities, or sensory loss. These compensations themselves may increase pressure load on specific regions.
Predicting Recurrence Risk (Vigilance Even After Healing):
For patients with a history of foot ulcers, even if the ulcer has healed, the original site or adjacent areas often remain biomechanical weak points. The pressure plate can continuously monitor whether the pressure in these areas has been effectively reduced by interventions (such as insoles, orthopedic shoes), or whether high-risk pressure still exists. Persistent, unresolved high pressure is one of the strongest predictors of ulcer recurrence.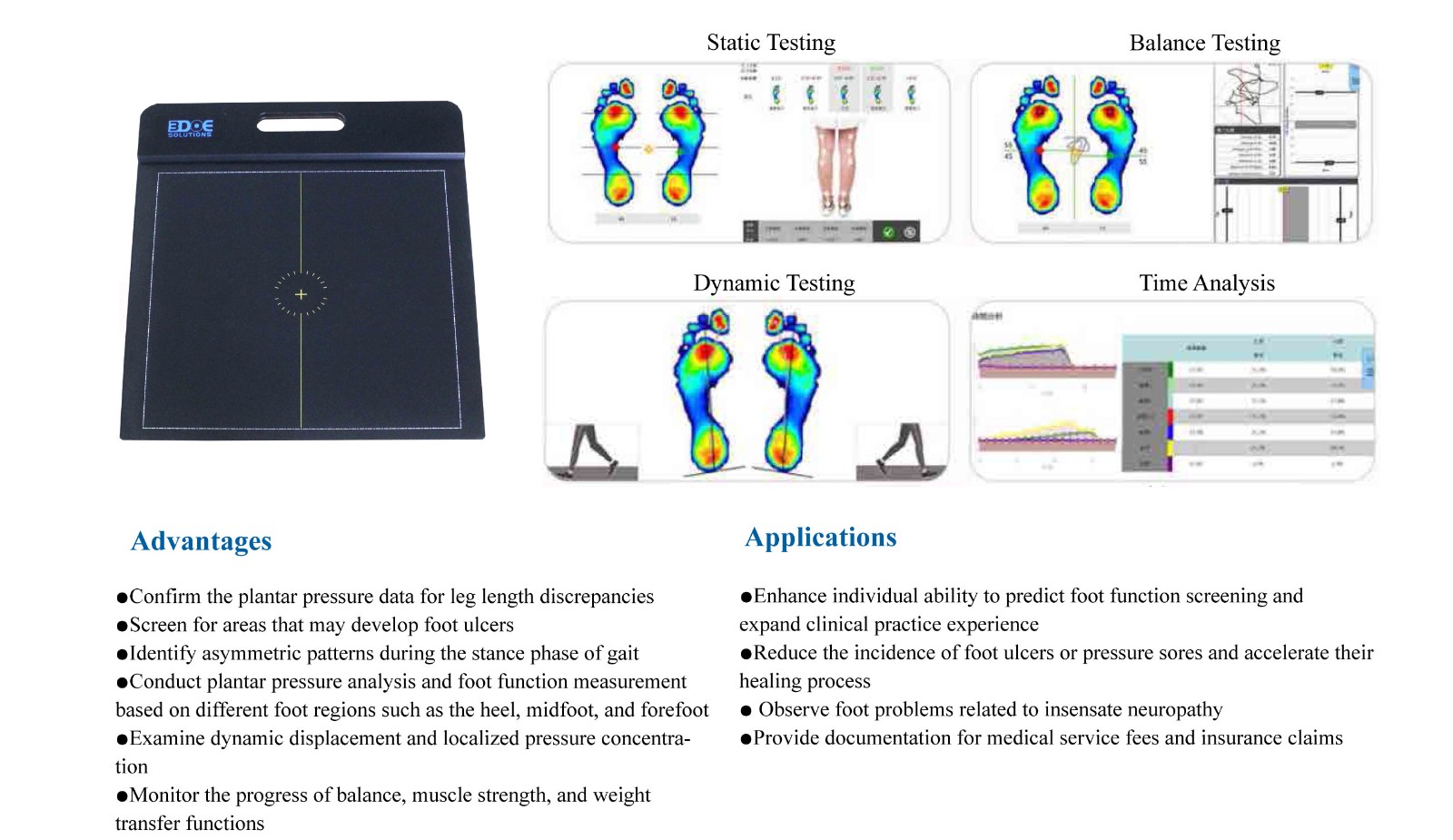
It can also evaluate whether the current offloading measures (such as custom shoes, insoles) achieve the intended effect.
Guiding Precise Intervention (From Prediction to Prevention):
Foundation for Personalized Offloading Plans: The detailed pressure distribution map provided by the pressure plate is the gold standard for designing customized orthotic insoles or therapeutic shoes. Engineers or orthotists can precisely design and place cushioning materials, support structures (such as metatarsal pads, arch supports), or modify the outsole (such as rocker bottom) on the insole, based on the exact location, range, and values of high-pressure points, to maximally disperse pressure and protect high-risk areas.
Basis for Gait Retraining: Physical therapists can use real-time feedback provided by the pressure plate (COP trajectory, pressure distribution changes) to guide patients in gait retraining, learning safer walking patterns (such as adjusting stride length, walking speed, and foot landing sequence), thereby reducing the duration and intensity of high-pressure loading areas.
Selection of Suitable Footwear and Socks: Test results can guide the choice or modification of ready-made shoes and socks, ensuring they provide sufficient space (avoiding compression of deformed sites) and cushioning (especially in high-pressure areas).
Behavioral Recommendations: Combined with pressure–time integral data, more targeted activity recommendations can be given, such as avoiding continuous walking beyond a specific duration to prevent excessive cumulative pressure on certain regions.
Key Considerations in Clinical Application:
Priority for Dynamic Testing: Dynamic pressure testing during walking reflects real plantar load conditions better than static standing tests, and thus has higher predictive value.
Standardization and Normalization: Testing is usually required to be performed barefoot, to eliminate the influence of footwear. Standardized testing protocols (walking speed, number of steps, etc.) should be followed.
Comprehensive Assessment: Pressure data is core, but ulcer risk prediction must be multimodal and multifactorial. It must be combined with:
Neuropathy assessment (e.g., 10 g monofilament, vibration sense, nerve conduction velocity).
Vascular status assessment (e.g., dorsalis pedis pulse, ABI, TcPO2).
Foot structure examination (deformities, calluses, previous ulcer scars).
Skin condition assessment.
Patient medical history (glycemic control, history of ulcers/amputations).
Regular Monitoring: The risk status of diabetic foot is dynamically changing (progression of neuropathy, changes in foot morphology, vascular status changes). Regular plantar pressure testing (every 6–12 months, or more frequently depending on risk level) is crucial for timely adjustment of interventions.
Individualized Thresholds: The pressure threshold for predicting ulcers is not absolutely uniform. It needs to be judged comprehensively by professional physicians based on the patient’s specific conditions (such as vascular status, tissue tolerance). Generally, peak pressure >700 kPa or significantly increased pressure–time integral is considered an important indicator of high risk, but interpretation must be individualized.

 +86-0755-86131192
+86-0755-86131192 2025-08-21
2025-08-21 Back to list
Back to list







 +86-0755-86131192
+86-0755-86131192